Analysis by
@jburnmurdoch
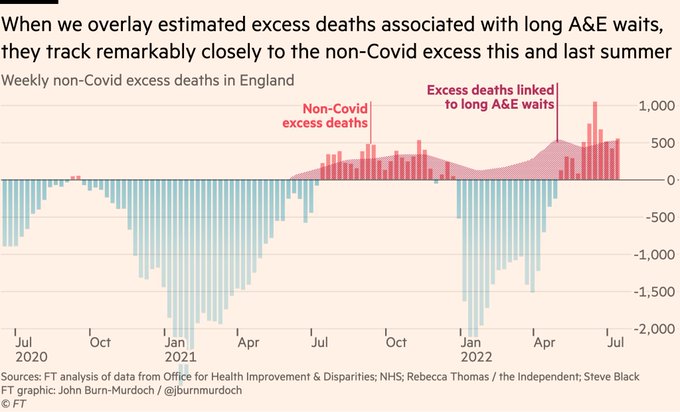
shows a fairly strong association between A&E waits and excess deaths this summer and last.
3
50
231
Replies
This rhetoric is divisive and unhelpful, particularly the headline.
It’s correct to say we are experiencing significant excess deaths. It’s also correct that much of the excess didn’t arise directly from COVID.
But I disagree with calling these deaths “lockdown effects”. 🧵
145
438
1K
We have been experiencing significant excess deaths for around three months now, as I have highlighted each week.
Some of the excess is explained by the ageing population, but the CMI’s age-standardised calculation still shows significant excess deaths - over 11,000 this year.
3
43
191
A significant proportion of the age-standardised excess are deaths with COVID.
However, a similar number are not. It is these non-covid deaths that
@sarahknapton
’s article focuses on, calling them “lockdown effects”. This attribution is speculative and I’d say it’s inaccurate.
14
38
318
To state the obvious, we have not been in lockdown for a long time. It is over a year since the last restrictions were lifted. We saw excess deaths after restrictions were lifted last July and we are seeing them again now.
So what are the causes of the “non-covid” excess deaths?
9
40
270
One useful source is the data from
@OHID
. This isn’t perfect - for example it would benefit from more granularity and full age-standardisation - but it’s enormously helpful. Much of the excess arises in cardiovascular conditions and diabetes.
@RichardLWeiss
@COVID19actuary
@actuarynews
Heart attacks and other cardiovascular issues are a major source of recent excess deaths.
See charts below from
@OHID
.
Source:
4
6
17
3
38
194
So what are the underlying causes? I think three main factors:
1. elevated cardiovascular risks after covid infection
2. current delays for urgent treatment in the NHS
3. missed and delayed diagnoses early in the pandemic
55
81
488
1. This recent article by
@saimamaysidik
in
@Nature
gives a good summary of concerns around post-COVID cardiovascular risk:
“studies suggest that the risk of cardiovascular problems, such as a heart attack or stroke, remains high even many months after a SARS-CoV-2 infection”
10
46
247
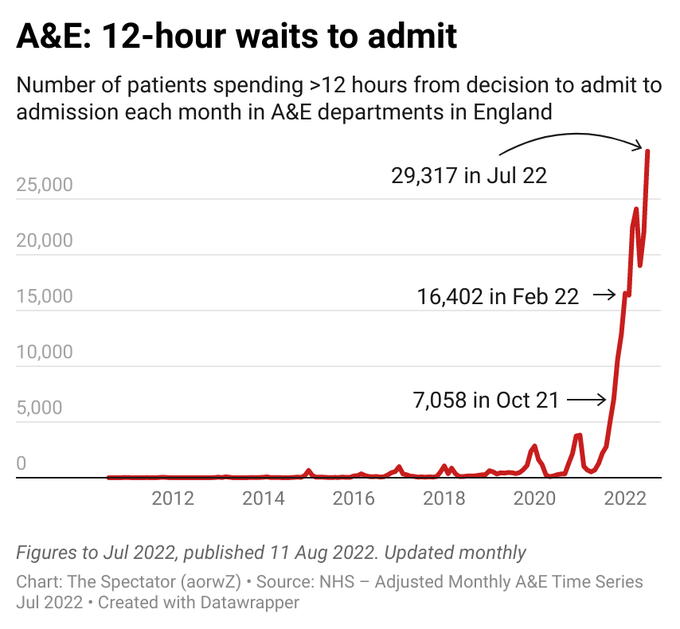
2. Current delays for urgent NHS care are extraordinarily long.
See chart below for those waiting >12 hours in A&E for example. Ambulance waiting times and other statistics are equally concerning.
Staffing levels, ability to discharge patients and demand are all relevant here.
2
34
217
3. Both the pandemic itself and our response to it have led to missed screenings and early diagnosis of various diseases. Missed or late diagnosis will lead to higher death rates.
8
20
177
It is only this third element that can reasonably be called “lockdown effects”. Even here though, many would argue that with no restrictions an overwhelmed NHS would have led to more missed or late diagnoses, as well as more short-term deaths.
7
21
268
We do not currently have data that allows us to investigate the breakdown between the 3 underlying causes discussed above. This is why the investigation referred to in the article (which I expect to contribute to) will happen. It is wrong to speculate on its outcome now.
5
14
152
For a more nuanced discussion of the indirect impacts of the pandemic see this recent
@COVID19actuary
bulletin by
@pearsonstuttard
and Melissa Shaw. /end
19
29
180
I missed this helpful reply earlier from the author of the article.
Sarah confirms here that the article does not mean what the headline (and first paragraph, and Telegraph tweets) suggest. “Feared” is not the same as “believed” etc.
@ActuaryByDay
It’s very clear we say it is ‘feared’ they are and ‘may’ be and that the government is looking into whether they are. We make it plain in the jumbo analysis inside other factors could be at play.
15
2
14
8
8
67
This thread from
@john_actuary
examines the numbers in more detail, forming a good companion piece to mine.
4
1
27
@ActuaryByDay
@jburnmurdoch
You might be interested in this:
'For every 82 admitted patients whose time to inpatient bed transfer is delayed beyond 6 to 8 hours from time of arrival at the ED, there is one extra death.'
1
0
1